Zurich Refuses to Pay for Emergency Treatment
In a medical emergency, a doctor treats first and asks questions later. But in response to a medical emergency, Zurich refused to pay a doctor for suturing a lacerated finger.
Zurich denied reimbursement for this emergency treatment, even after the provider obtained retrospective authorization.
The events unfolded as follows:
- The provider sutured an injured worker’s lacerated finger.
- The provider submitted an original bill for the emergency treatment.
- Zurich denied payment for the original bill as unauthorized emergency treatment.
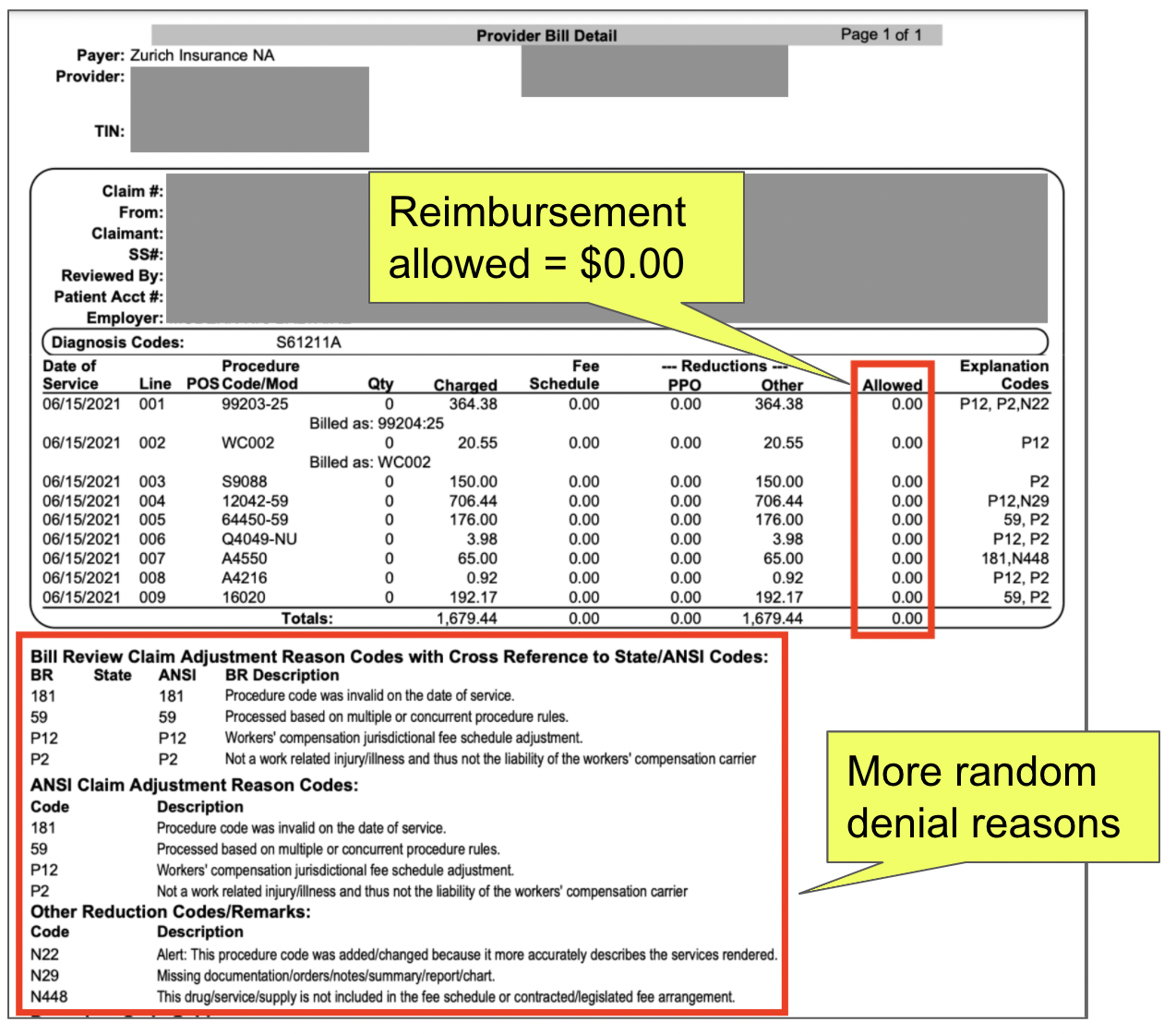
- The provider submitted a retrospective Request for Authorization (RFA) to Zurich for the emergency treatment.
- Zurich approved the emergency treatment specified in the RFA.
- The provider submitted a Second Review appeal disputing the initial denied payment.
- Again, Zurich denied payment.
- The provider paid $180 to request Independent Bill Review (IBR), in the hopes that California’s designated IBR entity, Maximus, will force Zurich to pay for the authorized emergency treatment.
Like so many wasteful disputes, it begs the question: why would any sane doctor treat injured workers? Repeatedly, we find evidence that bearing the administrative costs required to obtain proper reimbursement is financial masochism for California providers.
Zurich’s refusal to reimburse a doctor — even after the doctor received Zurich’s retrospective approval — makes one of the most compelling cases yet for much-needed workers’ comp reform.
Doctor Treats Lacerated Finger
When the worker came to the doctor with a lacerated finger, there was no time to fill out a formal RFA form or wait around for Zurich’s Utilization Review (UR). Instead, the doctor simply sutured the bleeding wound, with the expectation of reimbursement for emergency treatment.
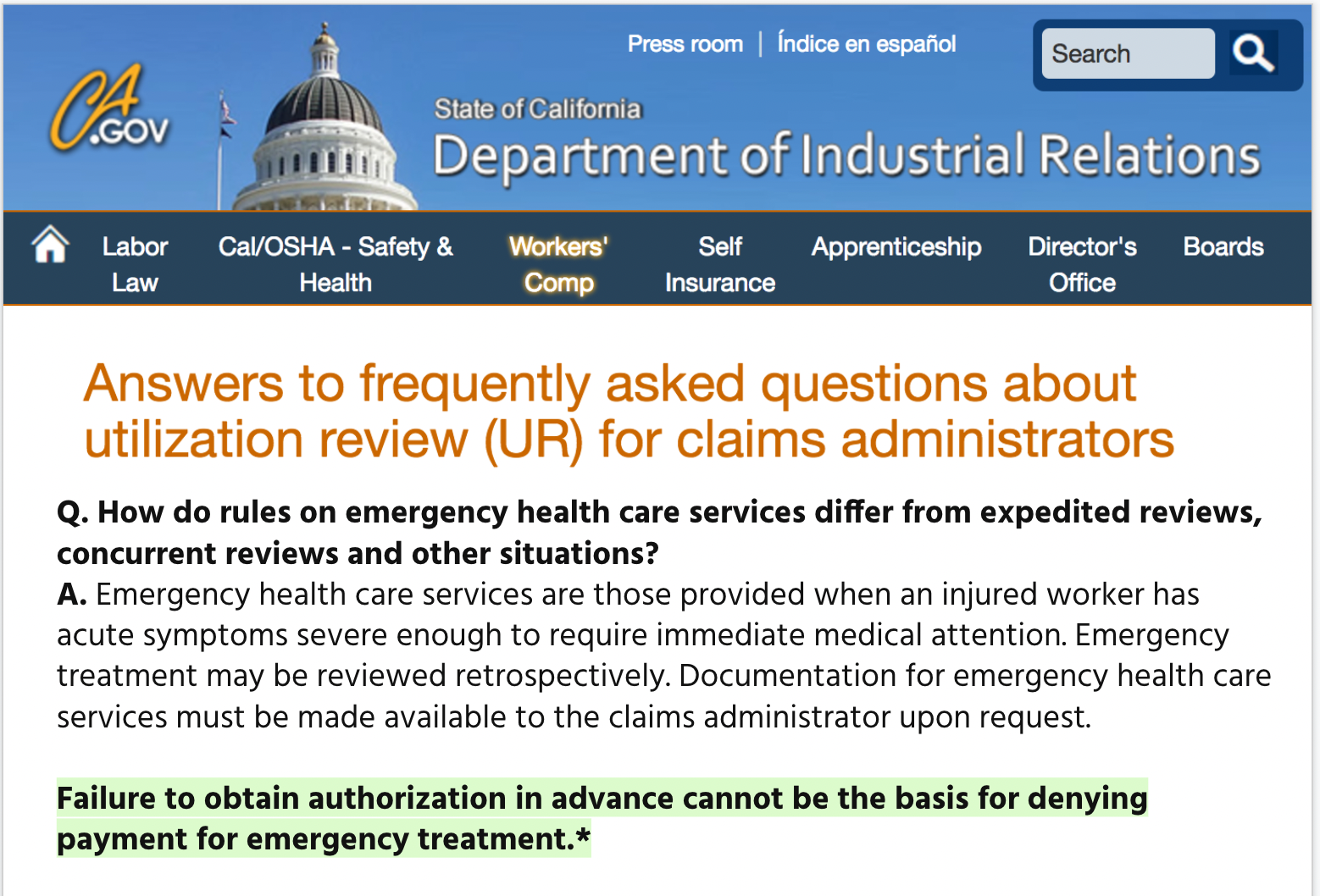
It’s a reasonable expectation. The Division of Workers’ Compensation (DWC) website instructs that “Failure to obtain authorization in advance cannot be the basis for denying payment for emergency treatment.”
*Emphasis added.
Zurich Denies Payment For Lacerated Finger
Unfortunately for the provider, Zurich is responsible for this injured worker’s care, and refused to pay the doctor for treating the lacerated finger.
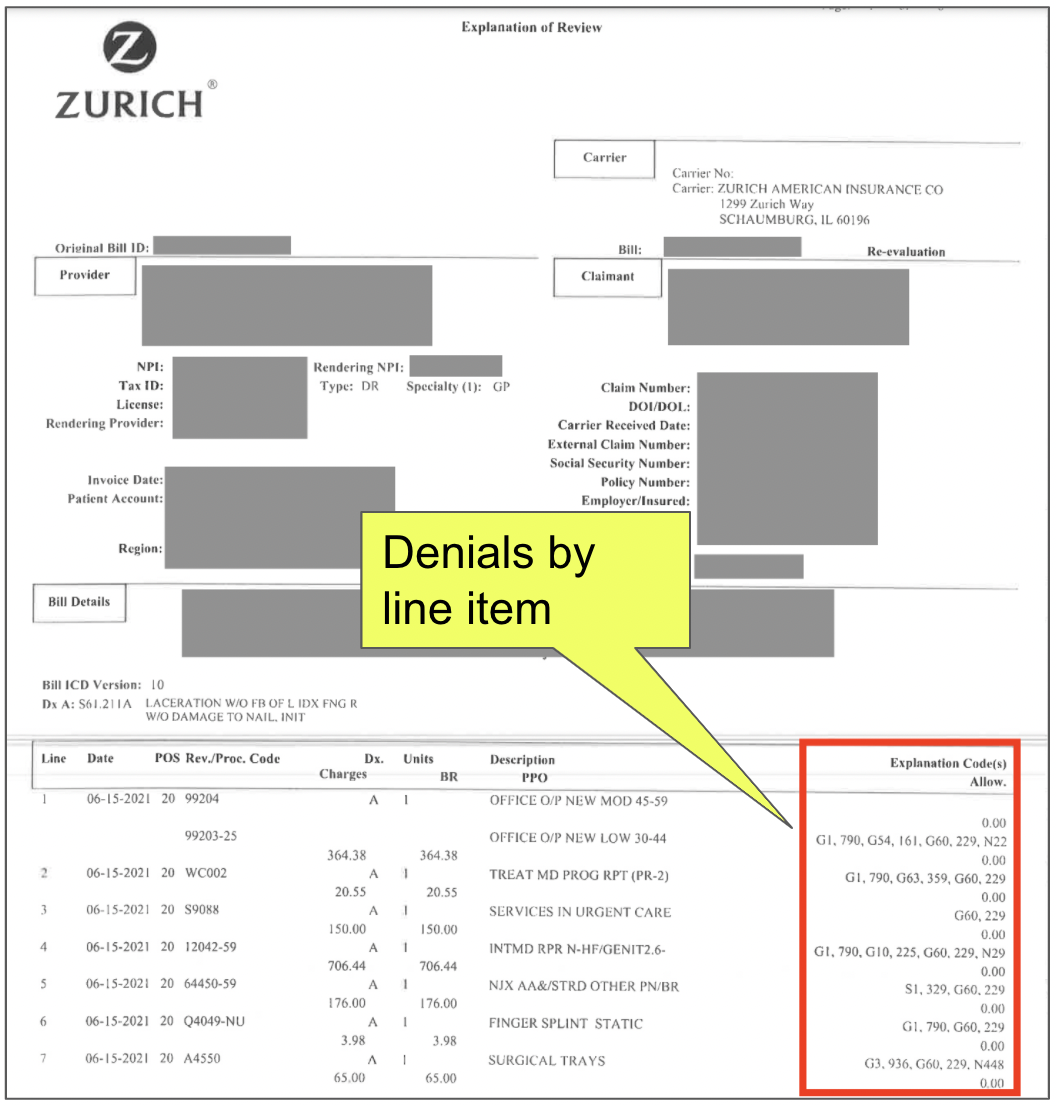
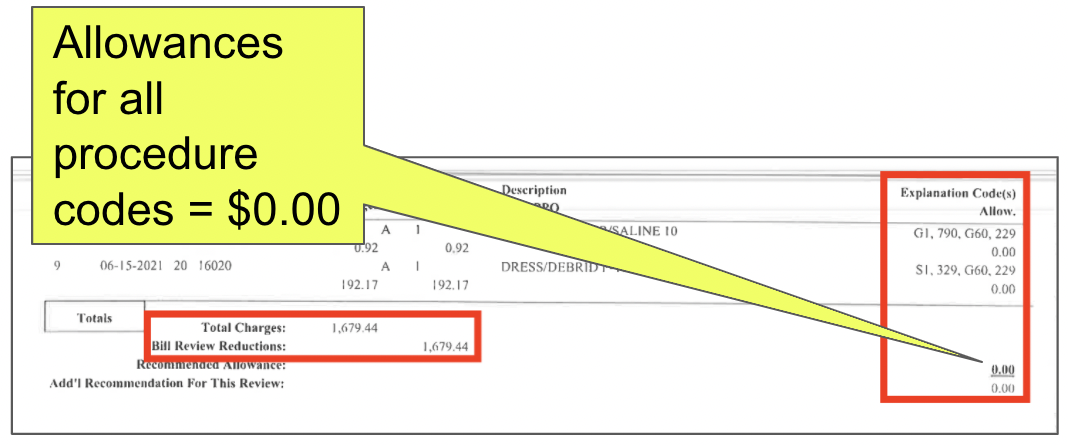
First, Zurich denied the original bill with a string of nonsensical reasons. The Explanation of Review (EOR) from Zurich (below) reads like a Mad Libs of denial codes, seemingly added to the document at random:
- “PAYMENT FOR THIS SERVICE HAS BEEN DENIED BECAUSE IT APPEARS TO BE UNRELATED TO THE CLAIMED WORK ILLNESS OR INJURY.”
- “THE SUBMITTED DOCUMENTATION DOES NOT SUPPORT THE SERVICE BEING BILLED FOR.”
- “THIS CHARGE DOES NOT APPEAR RELATED TO THE INJURY.”
Zurich Retrospectively Approves Emergency Treatment
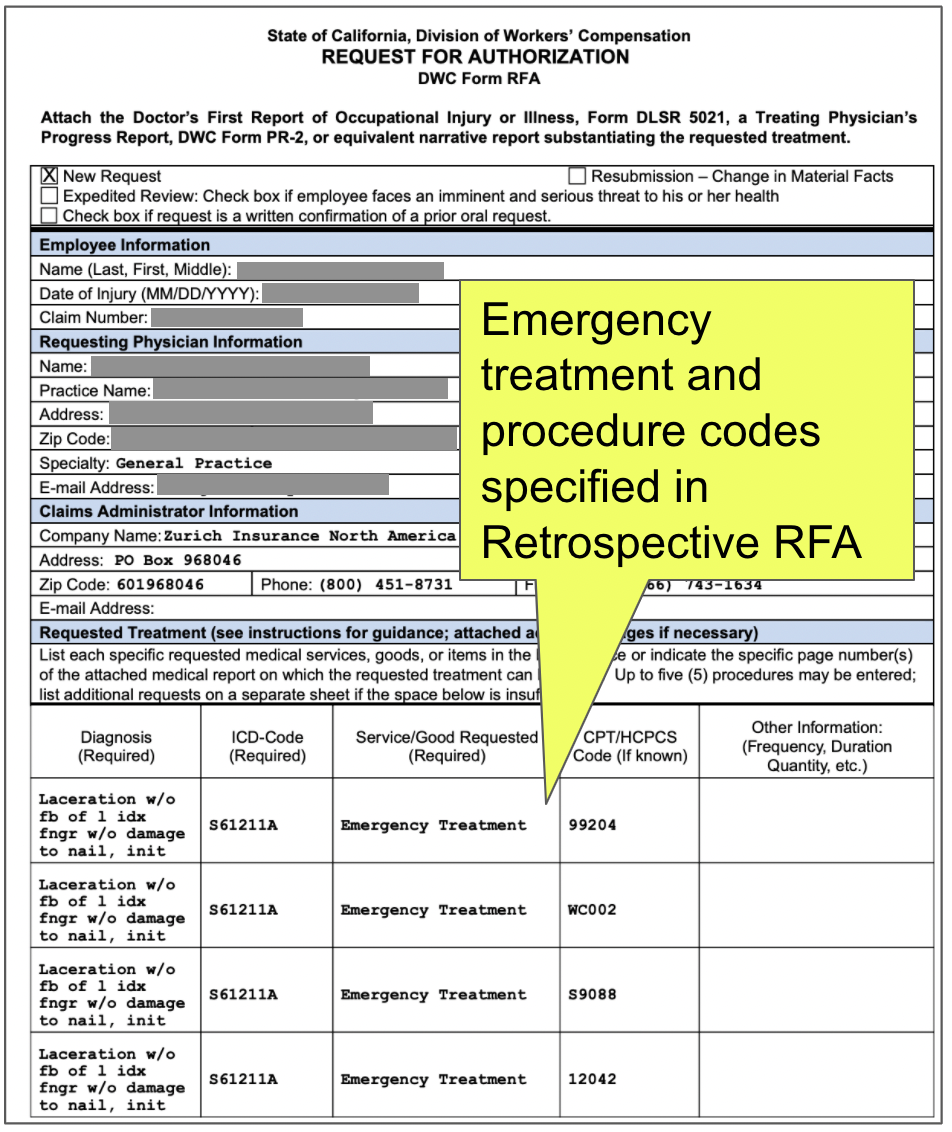
By denying payment for the emergency treatment, Zurich forced the doctor to submit a retrospective RFA (below) specifying precisely the emergency treatment rendered, right down to the procedure codes.
Remember, there are no mystical RFA fairies. Zurich’s denying payment for the emergency treatment meant the provider needed to expend even more administrative costs to submit the retrospective RFA to receive payment for suturing a wound.
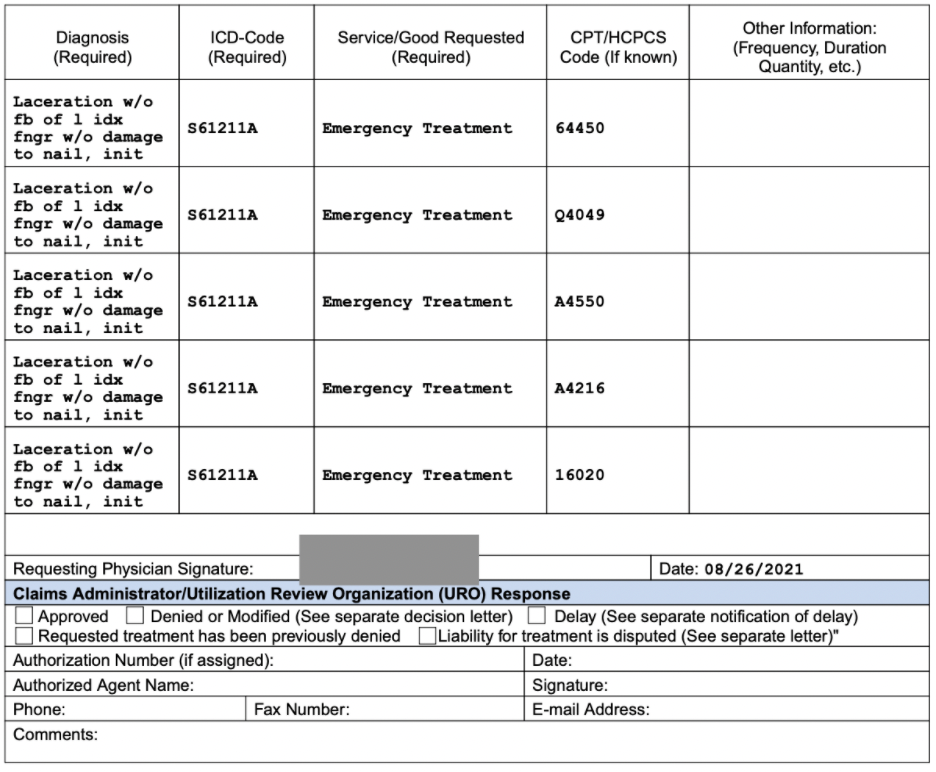
Zurich Approves Emergency Treatment
AGAIN, Zurich Denies Payment For Lacerated Finger
The doctor submitted a Second Review appeal disputing the initial denial of reimbursement. Included with the appeal was the above authorization for the services in question.
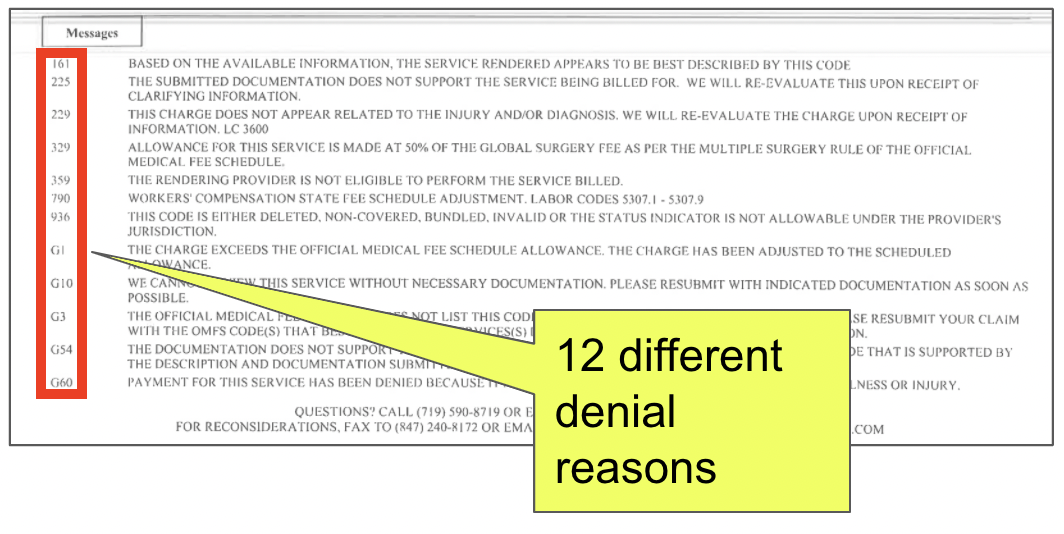
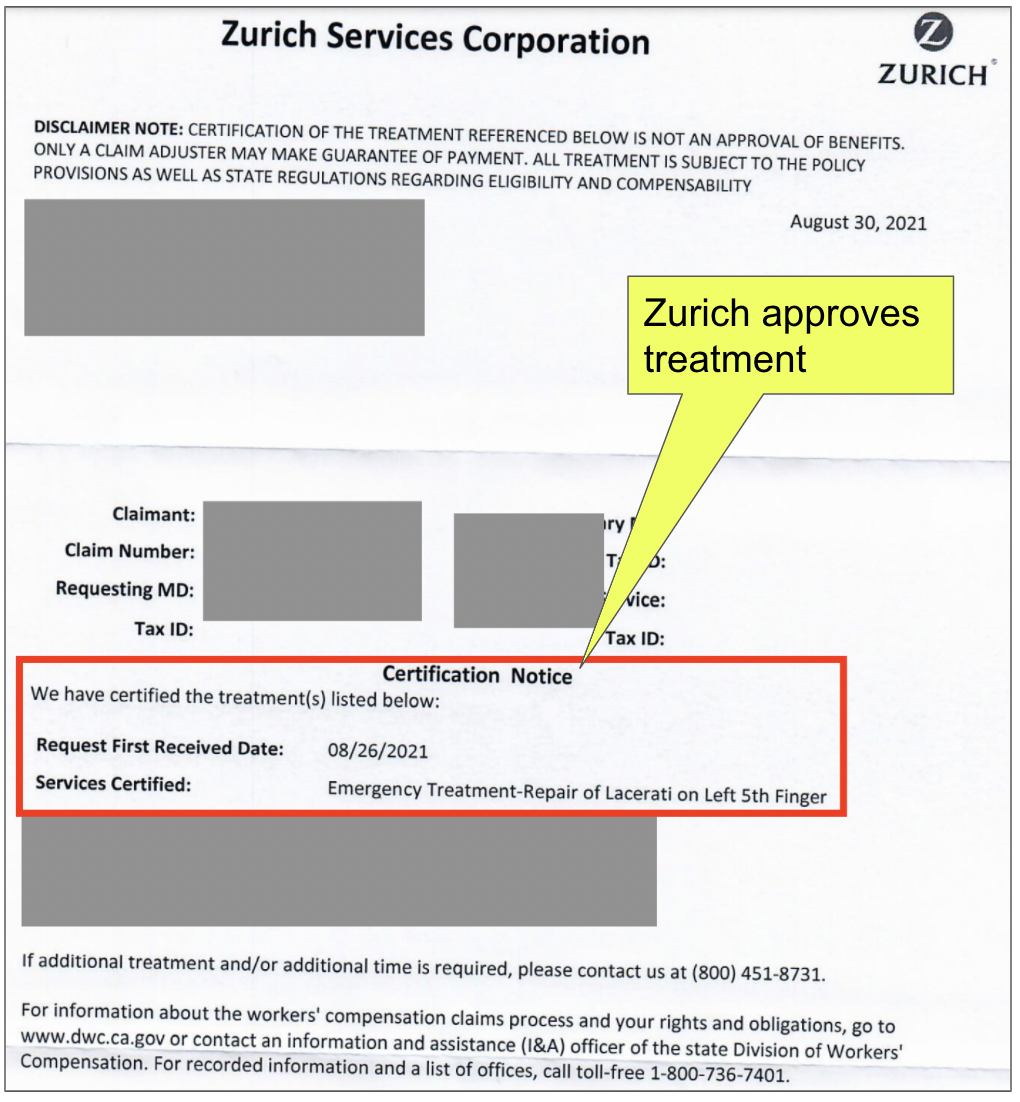
Zurich disregarded its own authorization and denied payment a second time, returning a final EOR (below) with another random assortment of denial reasons. This “everything bagel” of reasons not to properly reimburse the doctor included:
- “Procedure code was invalid on the date of service”
- “Workers’ compensation jurisdictional fee schedule adjustment”
- “Not a work related injury/illness…”
Provider Pays $180 To File For IBR
The second erroneous denial left the doctor with no choice but to request Independent Bill Review (IBR). The provider must pay $180 and file the IBR request within 30 days of receipt of the EOR.
As Zurich demonstrates, treating injured workers emergently is economically risky for providers. And that’s bad for all concerned.
This broken workers’ comp system empowers Zurich to choose whether to reimburse a doctor. In effect, authorization is not a guarantee of payment. When Zurich chooses not to reimburse a doctor, the doctor must embark on an extraordinarily expensive administrative journey to demand payment.
Now, California IBR will have to untangle this dispute.
Hopefully, the DWC will recognize Zurich’s denials for what they are: improper and invalid. Authorization is supposed to guarantee payment. But as we’ve learned before, that’s only true if the powers that be are willing to uphold the rules.
Get paid in full and on time — without the hassle. DaisyBill makes authorization, billing, and appeals quicker, easier, better. Reach out to see how our software and services can help your practice.
CONTACT US
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.