CA: New DWC Form 7 Warps Workers' Comp Reality
.gif)
California’s Division of Workers’ Compensation (DWC) announced an update to the DWC 7, one of many mandated workers’ comp forms.
Employers must, by law, display the information on the DWC 7 in a “conspicuous location frequented by employees” to inform those employees of their rights in the event of a work-related injury.
However, despite changes to the form necessitated by recent legislation, the new DWC 7 continues to mislead injured workers (and many physicians) by asserting that injured workers can expect the medical care recommended by their treating physicians to be immediately authorized (subject to a $10,000 cap).
California law does mandate that within one day of a worker’s report of an injury, the workers’ comp claims administrator must authorize all medically necessary care up to $10,000, regardless of whether or not the employer ultimately accepts liability for the injury.
However, another mandatory DWC form, the DWC 1, reveals the dark truth of the state’s barely governed workers’ comp system: claims administrators often do not authorize the care a newly injured worker needs. The DWC 1 form actually instructs injured workers to plead for authorization and, if pleading fails, to use their private health insurance or seek free care.
As all California workers’ comp physicians (should) know, claims administrators may deny payment for unauthorized care. Providers should not be fooled into believing the $10,000 myth promulgated by the DWC 7 form. Providing care to a newly injured worker without authorization is simply providing free care.
CA Payers MUST Authorize Care (Unless They Just Don’t Want To)
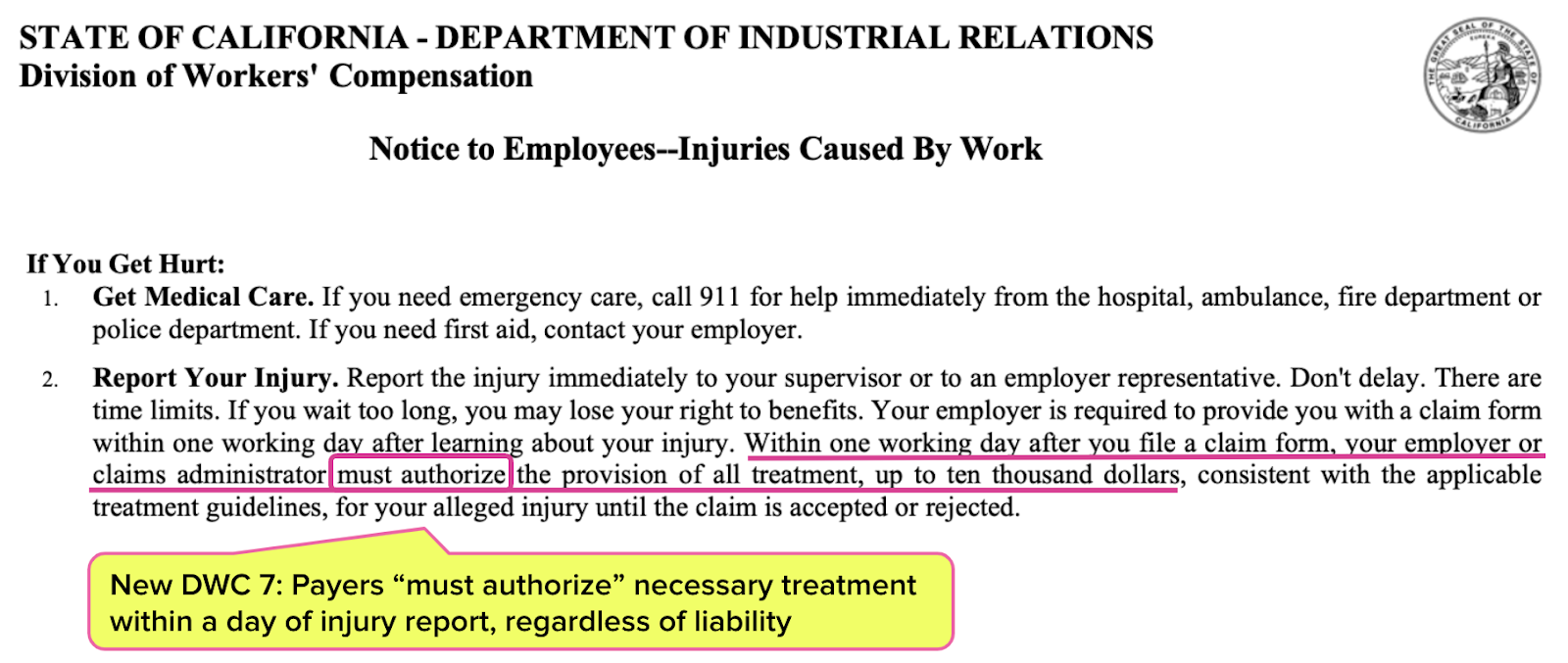
Both the current and the new version (shown below) of the DWC 7 propagate the myth that in the event of an injury, the workers’ comp claims administrator “must authorize” the provision of up to $10,000 worth of medically necessary and appropriate treatment within a single working day.
This supposed requirement addresses the fact that injured workers often need treatment before the claims administrator decides whether or not to accept liability for the injury as work-related. Since the claims administrator may take up to 90 days to make their liability decision, Labor Code Section 5402 instructs that necessary treatment be authorized in the meantime. The DWC 7 reflects this.
However, the DWC 1 tells a different story, which reflects the reality that defies the law.
As shown below, the DWC 1 is the mandated form an injured worker must use to file their claim with the employer. The DWC 1 explains that in practice, the claims administrator can refuse to authorize treatment until liability for the injury is decided.
As we’ve decried before, the DWC 1 instructs injured workers that if the employer or claims administrator refuses to authorize care, “Ask for treatment to be authorized right now.”
Next, the DWC 1 instructs the injured worker that if the employer refuses to authorize care, the worker must obtain care themselves by either:
- Using their private healthcare insurance (which may or may qualify as an act of insurance fraud, since it’s illegal to use private insurance to cover work-related injuries), or
- Finding a free clinic
To repeat (to ensure this fact sinks in): on the mandated form an injured worker files with their employer, the DWC instructs that claims administrators may ignore the law requiring that up to $10,000 in treatment be authorized, so finding (and paying for) care is the injured worker’s responsibility.
In other words, the DWC 1 form shows that the DWC 7 is inaccurate and arguably misleading to injured workers and their physicians. The DWC 7 lulls California workers into believing their employer will pay for their treatment—until they get hurt at work, and the DWC 1 treats them to a shocking dose of reality.
While the DWC is fine with misguiding California workers, providers should not fall prey to this bait-and-switch tactic. Providers should know the dangers of treating an injured worker without the claims administrator’s authorization, because unauthorized care is FREE care.
Submit RFAs in 30 seconds and automatically track UR decisions with daisyAuth. Request a demo below!
GET A DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.