DWC's Updated IBR Form - F Is for Fail

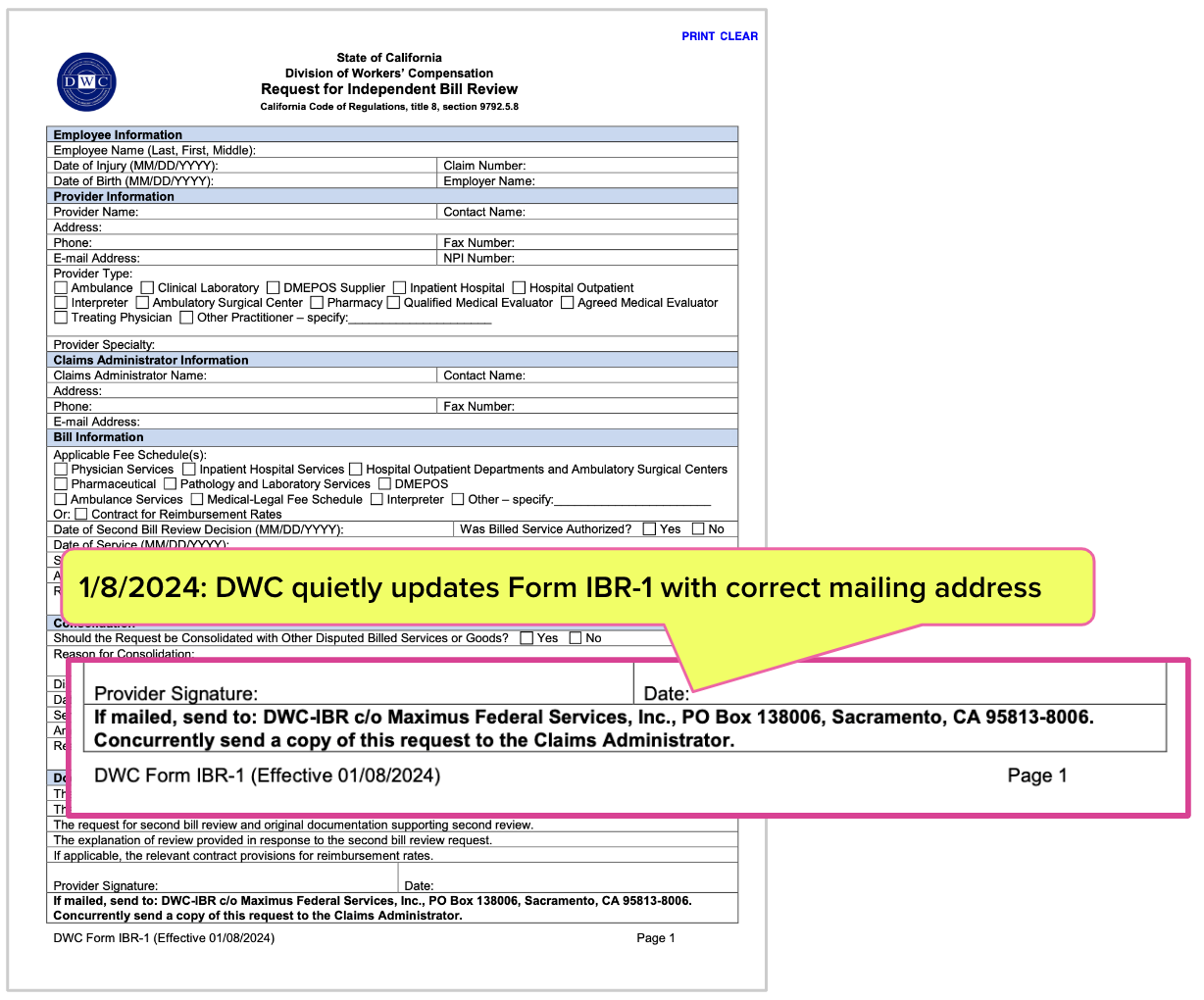
California’s Division of Workers’ Compensation (DWC) recently updated Form IBR-1, which providers use to request an Independent Bill Review (IBR)—but did so without publicizing the changes or correcting other long-standing errors on the form.
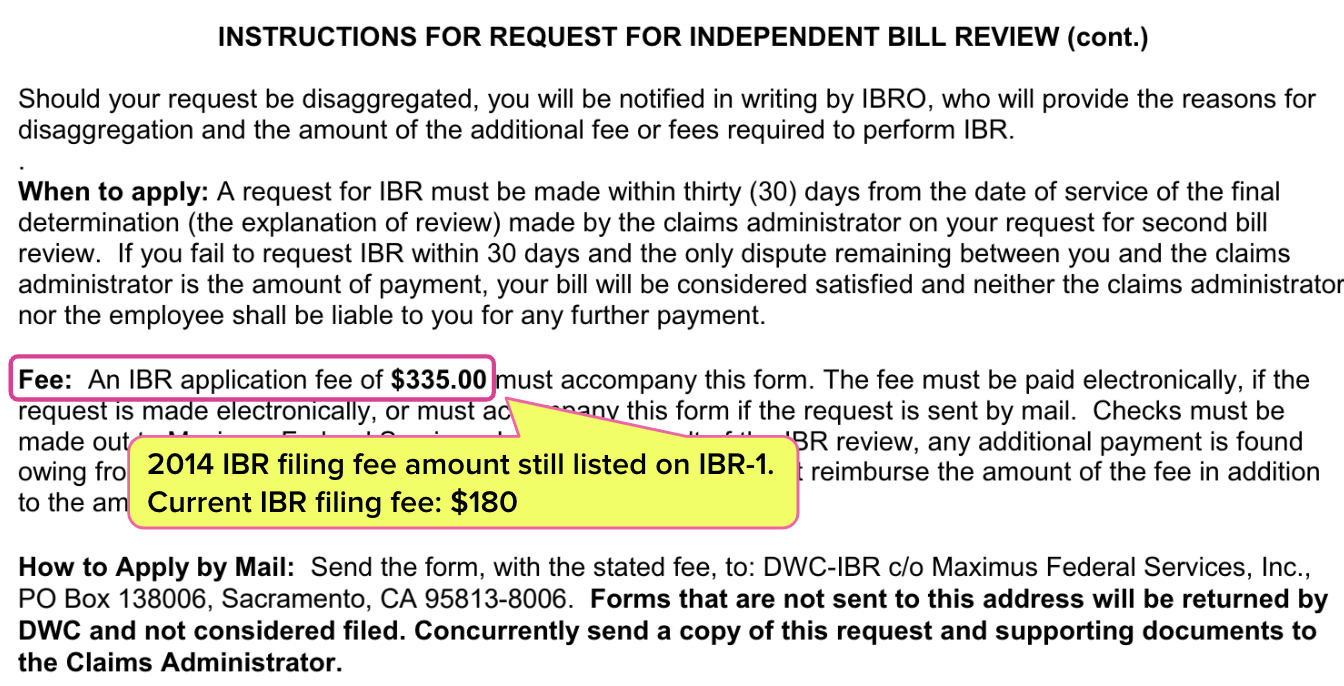
While the DWC updated the erroneous mailing address on the form, more critically, the form still lists an incorrect IBR filing fee amount of $335, despite the actual cost being $180. This filing fee error has persisted for over nine years.
For months, the form directed providers to send IBR requests to the wrong address. For years, it has inaccurately instructed providers to pay $335, causing confusion and potential financial loss. This IBR negligence by the DWC conveys a troubling message that providers are not the agency’s priority.
Instead, claims administrators and their private equity owners’ profits are seemingly the agency’s first concern. With little regulatory oversight, the DWC emboldens claims administrators to improperly pay providers, abandoning these providers to navigate the DWC’s flawed appeal system with insufficient guidance and support.
This IBR tale is yet another example of the many state-endorsed payment abuses inflicted on the providers who care for California’s injured workers.
IBR: A Regulatory Clown Show
The DWC has established a workers’ comp payment system that financially incentivizes claims administrators to issue payment denials and reductions inappropriately to providers.
When a claims administrator falsely denies or incorrectly reimburses a provider, the DWC makes the provider economically and administratively responsible for navigating the payment dispute process as follows:
- The provider must submit a timely and compliant Second Review appeal within 90 days of receipt of the incorrect payment.
- With the DWC’s blessings, the claims administrator may deny the appeal as a “duplicate” of the original bill.
- To dispute the improper Second Review denial, the provider must submit a timely and compliant IBR submission (complete with voluminous documentation) within 30 days and somehow know to pay $180 instead of $335 for the IBR.
Suppose a provider fails to properly or timely submit a Second Review appeal or IBR request. In that case, the DWC will rule the payment dispute ineligible for IBR and allow the claims administrator to retain the payment owed to the provider.
The DWC appeals process is riddled with financial pitfalls for providers, who must adhere to strict administrative requirements. If there is one mistake, the DWC allows the claims administrator to walk away with the payment rightfully owed to the provider.
Suppose a provider timely and correctly requests IBR; the DWC offers claims administrators even more protection:
- The DWC allows the claims administrator to simply pay the disputed amount without penalty or consequences after the provider requests IBR, but before the IBR is conducted—heads I win, tails you lose.
- The DWC allows the claims administrator to change the stated reason for the payment denial or adjustment. The claims administrator’s “updated” reason often involves a "threshold" issue around authorization or liability, allowing the DWC to step in and rule the dispute ineligible for IBR.
In effect, the DWC acts as the claims administrator’s “wingman,” intervening to protect the claims administrator while failing to provide even basic, correct appeal instructions to providers.
Finally, the DWC utterly fails to enforce the California law requiring the claims administrator to reimburse the $180 filing fee when the provider prevails at IBR. As a result, claims administrators routinely short providers the $180, even when IBR determines that the provider was correct.
New IBR Request Mailing Address
In September of last year, daisyNews reported that the mailing address listed on the IBR-1 had been incorrect for months.
Providers must request IBR within 30 days of receiving the final Explanation of Review (EOR) following a Second Review appeal. The incorrect address caused IBR requests to be returned to the provider as undeliverable, potentially making it impossible to submit the request within the mandated time frame—in effect, a financial gift to claims administrators courtesy of the DWC.
Half a year after changing the mailing address, the DWC finally updated the IBR-1. The correct address below now appears on the form:
DWC-IBR c/o Maximus Federal Services, Inc.
PO Box 138006
Sacramento, CA 95813-8006
To daisyNews’ knowledge, the DWC failed to alert the provider community to this mailing address correction. Rather than instructing providers to correct their IBR process, the DWC remained on-brand and kept providers in the dark.
DWC Leaves Stated IBR Filing Fee Incorrect
Despite making an effort to change the incorrect address on the form, the DWC failed to correct the amount a provider must pay to request IBR.
Initially, in 2014, the DWC required providers to pay $335 to file for IBR. In the last ten years, the DWC has changed the IBR filing fee twice:
- Effective January 1, 2015, the DWC reduced the fee to $195.
- Effective January 1, 2020, the DWC reduced the fee to the current rate of $180.
Yet even this latest version of the IBR-1 form lists the IBR filing fee as $335. The DWC has failed to correct an error that adversely impacted providers for nine years.
It is impossible not to believe that the DWC is choosing sides in payment disputes–and it’s not the providers’ side.
daisyBill makes treating injured workers easier, faster, and less costly. Request a free demonstration below.
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.





Fantastic write-up! Your insightful analysis of the DWC's updated IBR form highlights the critical gaps that need addressing. Your dedication to keeping us informed and your clear, concise writing style make complex topics accessible. Keep up the great work!