Liberty Mutual Feeds UR Vendors (While CA Worker Waits for Care)
In California workers’ comp, Utilization Review (UR) is the process by which claims administrators decide whether or not to authorize the care recommended by an injured worker’s treating physician.
UR is also a mess in California, with medically necessary and appropriate care delayed and denied over extended (7 years typically) and expensive injury claim durations—all while various entities profit from the administrative hurdles imposed on physicians attempting to treat injured workers.
For example, we recently reported how an injured worker went 23 months from the Date of Injury before receiving necessary surgery. Along the way, multiple UR vendors employed by Liberty Mutual compiled bloated, sometimes nonsensical UR decisions that seemed to be generated by an AI programmed with boilerplate UR language.
In this case, the employer apparently paid for two UR decisions—the initial denial and the later decision to approve the surgery despite little change in the case's material facts. The only result of needlessly delaying this injured worker’s care seems to have been getting multiple UR vendors paid twice.
MES, MediCall Deny Care on Behalf of Liberty Mutual
With 49 cents spent on administrative costs (like UR) for every dollar of actual benefits delivered to injured workers in California, there’s money to be made by vendors willing to take UR decisions off claims administrators’ hands, regardless of whether or not those decisions make sense.
Following the injury, it took an entire year (and a Medical-Legal dispute) for the worker to obtain permission to see an orthopedic specialist. After an initially conservative treatment approach failed, the orthopedist submitted Requests for Authorization (RFA) to Liberty Mutual recommending:
- Four surgical procedures
- Preoperative clearances
- Postoperative physical therapy
- A postoperative shoulder sling
- Postoperative pain medication
On November 20, 2023, Liberty Mutual responded with a 23-page tome (read it in full here if you dare), denying all of the recommended treatment above.
The treatment denial was the handiwork of two UR vendors, MES Peer Review Services and MediCall. MES denied all recommended treatments, with MediCall apparently (and redundantly) endorsing MES’s denial of the shoulder sling required for post-op rehabilitation.
Why did it take two UR vendors to deny the same sling?
Of note, the injured worker’s injury occurred in June 2022, and as of November 20, 2023, the injured worker had not been able to return to work. The medical documentation indicated that during those seventeen months, the injured worker's attempts at conservative treatment failed.
With denial of the recommended surgery, the injured worker would remain out of work, keeping the claim open and the employer paying for the foreseeable future.
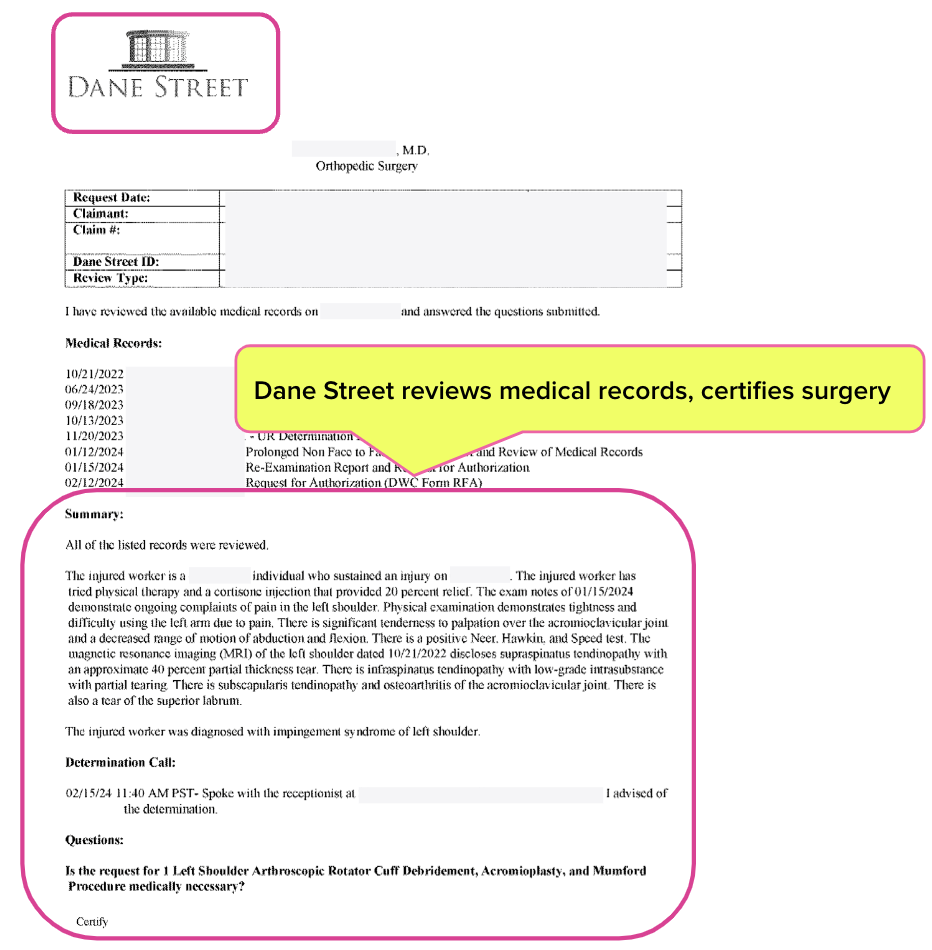
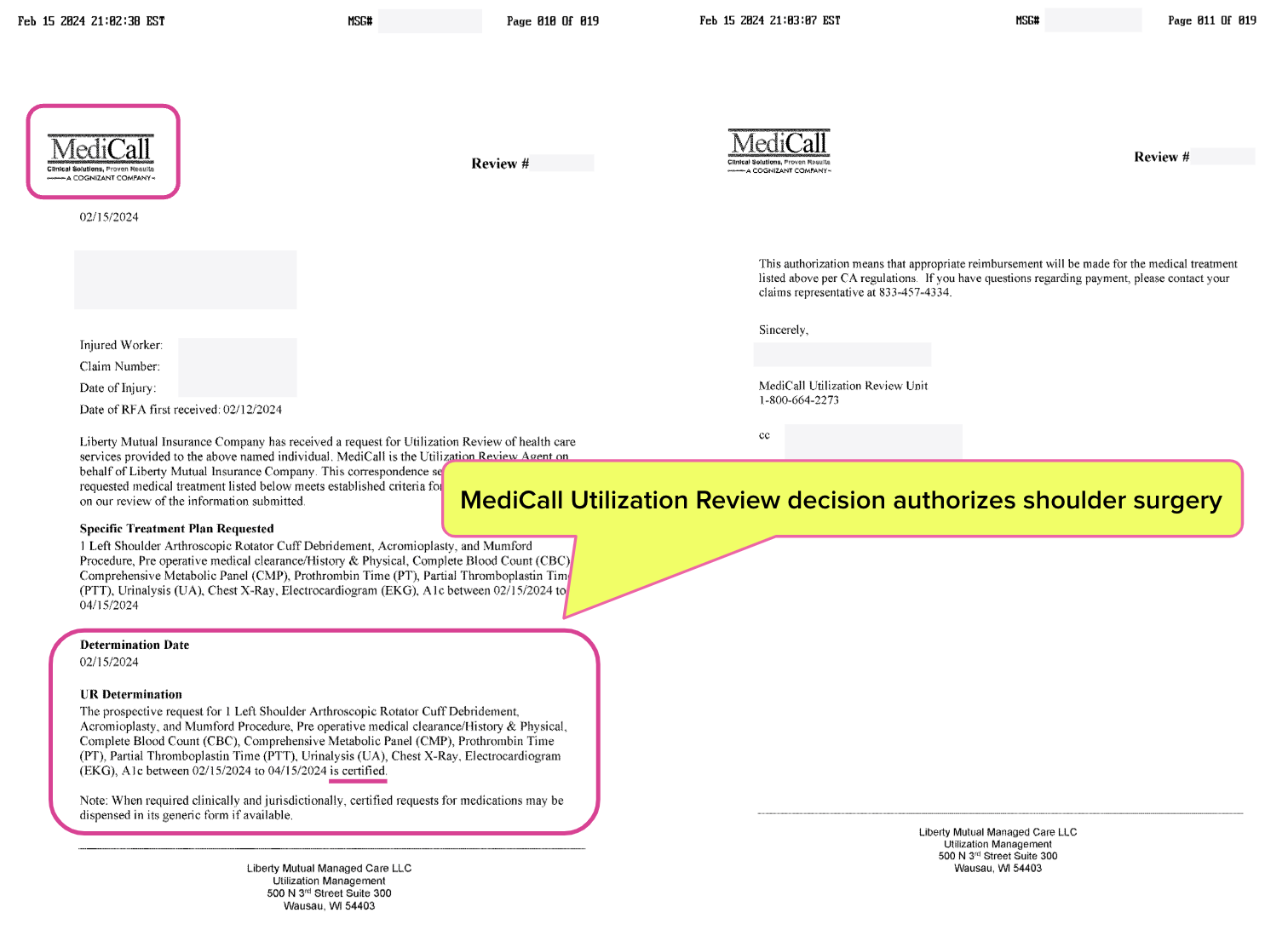
Dane Street, MediCall Approve Care on Behalf of Liberty Mutual
On January 15, 2024, the injured worker returned to the orthopedic surgeon with pain levels at 10 out of 10. After reexamination, the orthopedist again requested approval for surgery.
This time, Liberty Mutual responded with a 19-page UR decision approving the requests. The UR vendor was Dane Street, with another redundant assist from MediCall.
This is how the California UR system wastes employers’ workers’ comp dollars (albeit 49 cents at a time).
Had this worker received the care they needed sooner—without a Medical-Legal battle and without months of applying fruitless, “conservative” care over the treating physician's objections—this claim could have cost substantially less to resolve.
Employers pay to have their employees’ care restricted to Medical Provider Networks (MPNs), only to have UR vendors (which the employers also pay for) deny the treatments requested by MPN physicians, setting the stage for more doctor visits, more UR, and more money flushed.
It’s time to set the record straight regarding the most harmful misconceptions about UR and workers’ comp in general, and make it clear that:
- Doctors are NOT the ones wasting money (allegedly by over-diagnosing and over-treating) and
- UR denying care does NOT reduce employers’ workers’ comp costs.
All available data clearly demonstrate that employers' dollars are not “wasted” on treatment. Instead, their dollars are spent on adjacent costs like MPNs, UR, Medical-Legal battles, bill review, and every other obstacle to injured workers’ treatment and providers’ payment for that treatment.
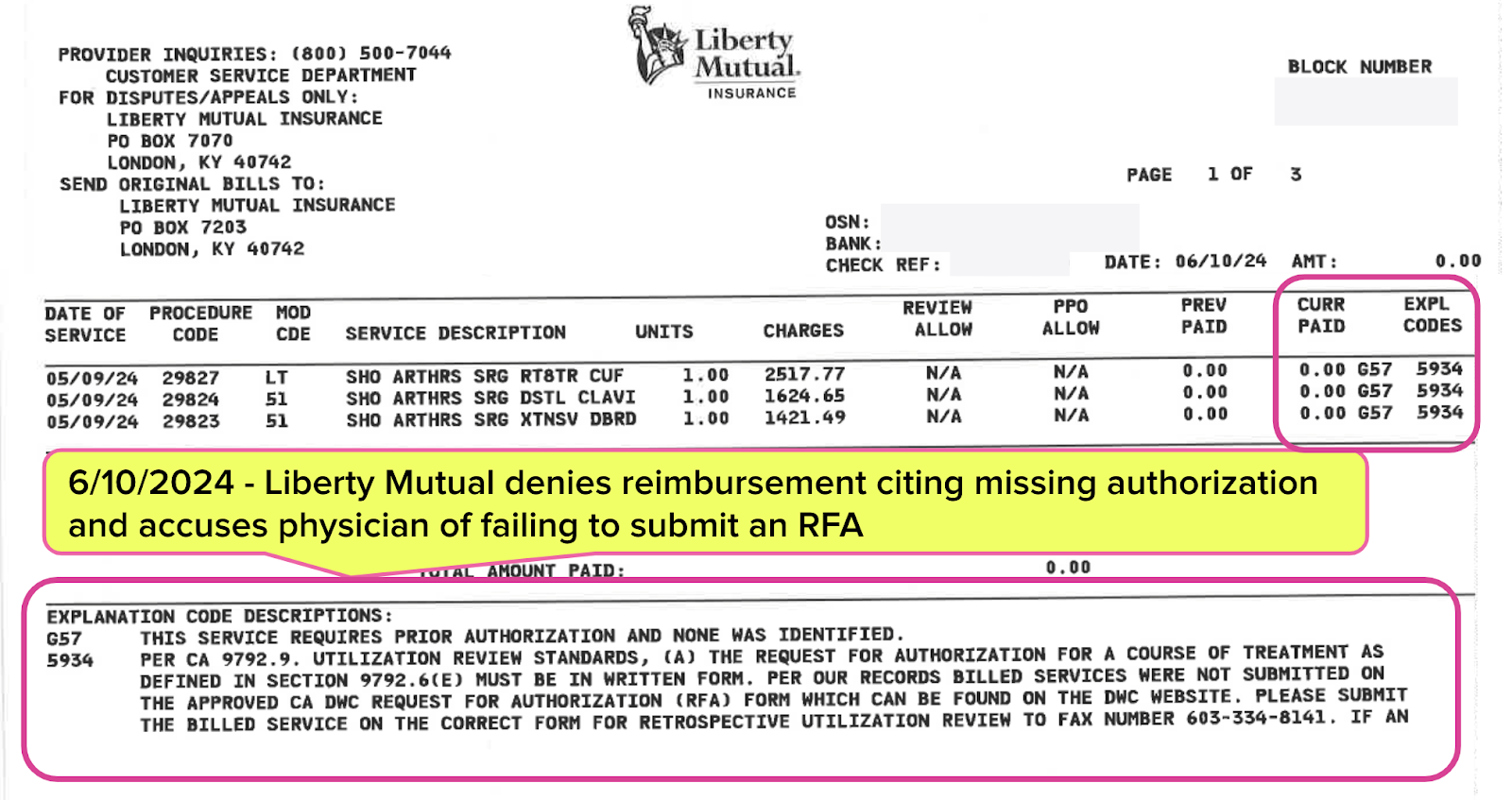
Spoiler: Liberty Mutual Refuses to Pay Orthopedist
The time and administrative effort this orthopedist expended simply to get authorization for surgery was extraordinary. Still, these efforts pale compared to the orthopedist’s hellish battles to get paid for that surgery.
In our next article, we’ll explore how Liberty Mutual refused payment for these authorized procedures (and how California’s Division of Workers’ Compensation (DWC) enabled this insurer’s indefensible behavior). Stay tuned.
Submit RFAs in 30 seconds and automatically track UR decisions with daisyAuth. Request a demo below!
REQUEST DEMO
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.


.gif)



.gif)
1, Workers compensation is a factory for chronic pain. 2. UR is completely broken. Recent example: requested a tube of Biofreeze for a patient with now chronic neck a shoulder pain. Received request for peer to peer. Really! My staff knows to grab me immediately to talk to the doctor, but it is never the doctor, but a staffer telling me to call back, never able to connect. Uggh! They wanted to know quantity. Huh? One tube, you can buy them at Walmart. Missed the "deadline" to discuss, request denied. On to IMR, costing the carrier hundreds of dollars instead of $14. On what planet does this make any sense?