Why Attorneys (and Providers) Can Trust daisyBill Fee Schedule Calculations
Recently, daisyNews addressed an unfounded and spurious accusation: that the reimbursement calculations provided by our Fee Schedule Calculator are unreliable due to some sort of bias in favor of providers.
This prompted several comments from readers, including defense attorneys who represent payers. Some came to dasiyBill’s defense, like the attorney who noted:
“I would leave a positive review for you if I knew where and how. I am a defense attorney who uses your OMFS calculator daily. Easy and accurate.”
Others had incisive but valid questions, like the attorney who wrote:
“I see a problem quite often when I use daisyBill for my calculations (I am on the defense side) and the provider claims to use daisyBill and their calculations differ! Why??? How does that happen?”
The above is a perfectly reasonable question posed in good faith — one we’re happy to answer in detail below.
Tl;dr: To arrive at identical reimbursement amounts, the provider and defense attorney must enter identical variables (place of service, date of service, county, etc) into the Fee Schedule Calculator.
Read on to learn more about these calculations, including how variables like National Correct Coding Initiative (NCCI) edits factor in.
Variables in Fee Schedule Reimbursement Calculations
As noted in our previous article, California’s Physician Fee Schedule is not simply a list of procedure codes and reimbursement amounts — if that were the case, there’d be no need for a Fee Schedule Calculator.
Instead, the Physician Fee Schedule comprises hundreds of pages of instructions for determining reimbursements based on a multitude of variables, including:
- The Date of Service
- The Place of Service Type (Facility or Non-Facility)
- The Provider Type (Physician, Non-Physician Practitioner, Social Worker, etc.)
- The Place of Service county or zip code for Geographic Practice Cost Indices (GPCI)
- The actual billing procedure codes (and modifiers, if applicable)
- The number of units of each procedure code
Each of the above variables can affect the reimbursement amount calculated.
If a provider and a defense attorney each use the Fee Schedule Calculator and generate different reimbursement amounts, it’s because the two parties entered different variables into the Calculator. For example, a commenting doctor noted:
“I see a problem as well when defense does not add in the correct amount of units (someone used one unit) hence, the allowance would be different when I would enter the correct amount of units as billed.”
Providers, bill reviewers, attorneys, and other stakeholders must agree upon the correct inputs to get objectively correct reimbursements. Once the six variables noted above are established (and in the case of a dispute, agreed upon by all parties), the Fee Schedule Calculator will do the math accurately.
NCCI Edits Explained - daisyBill Shows the Work
Moreover, while the variables listed above determine the “Base Maximum Fee” for each procedure code, other factors, such as National Correct Coding Initiative (NCCI) edits and other fee-affecting regulations, may come into play.
The defense attorney who was perplexed by differing Calculator results added the following to their comment:
“Also, many providers refuse to accept the NCCI edits when it reduces their reimbursement value.”
Medicare developed the National Correct Coding Initiative (NCCI) Edits, which apply to the California Physician Fee Schedule. These NCCI edits prevent payment when providers report improper code combinations or service units. While providers may wish to reject NCCI edits, doing so would contradict the fee schedule.
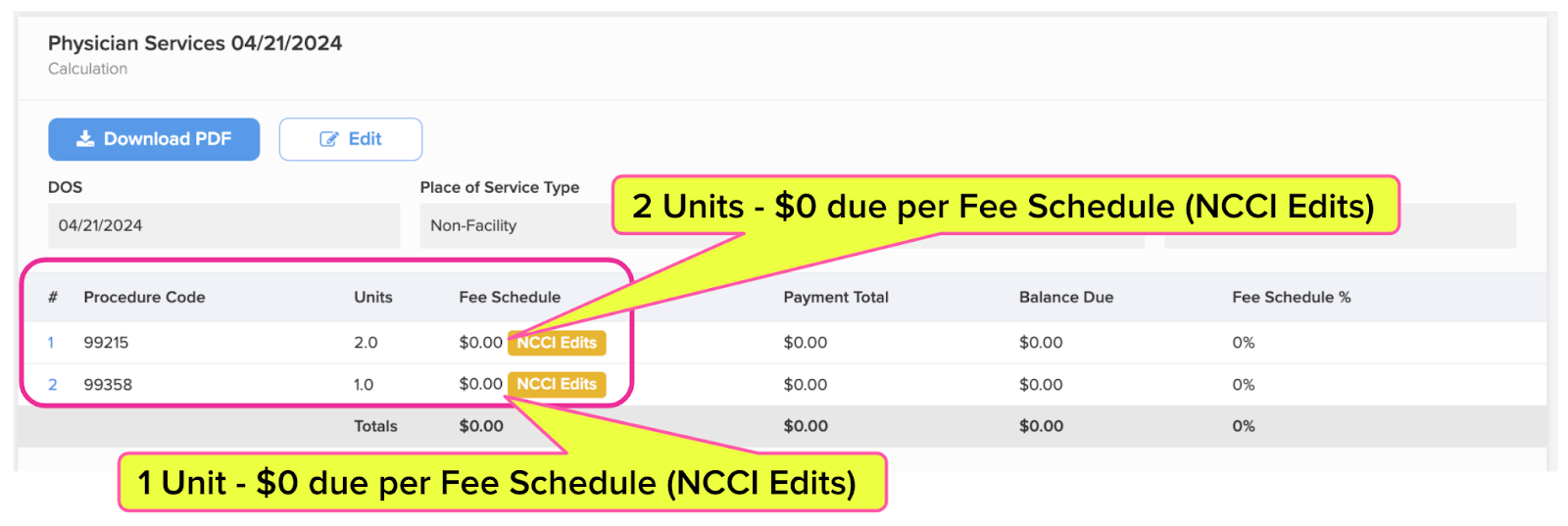
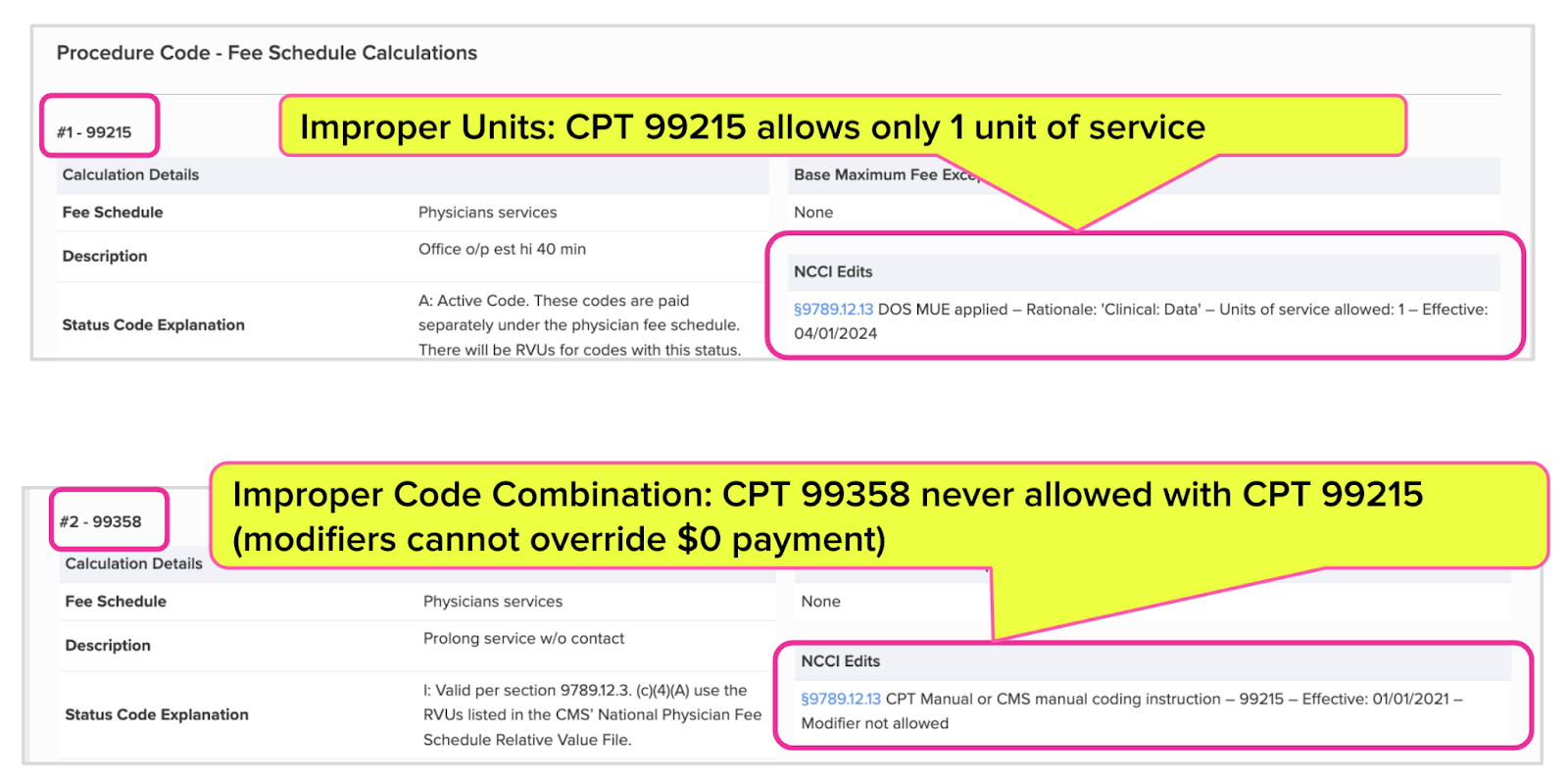
In the example calculation below, the NCCI Edits badge indicates that NCCI edits negate reimbursement for the two Procedure Codes listed: CPT 99215 for evaluation and management services and CPT 99358 for extended non-face-to-face time spent by a provider.
Our software does not ask anyone to take our word for its reimbursement calculations. In the “Procedure Code - Fee Schedule Calculations” section, the daisyWizard explains why the NCCI edits resulted in $0 reimbursements
- CPT 99215 - Improper Units; Units of service allowed: 1
- CPT 99358 - Improper Code Combination
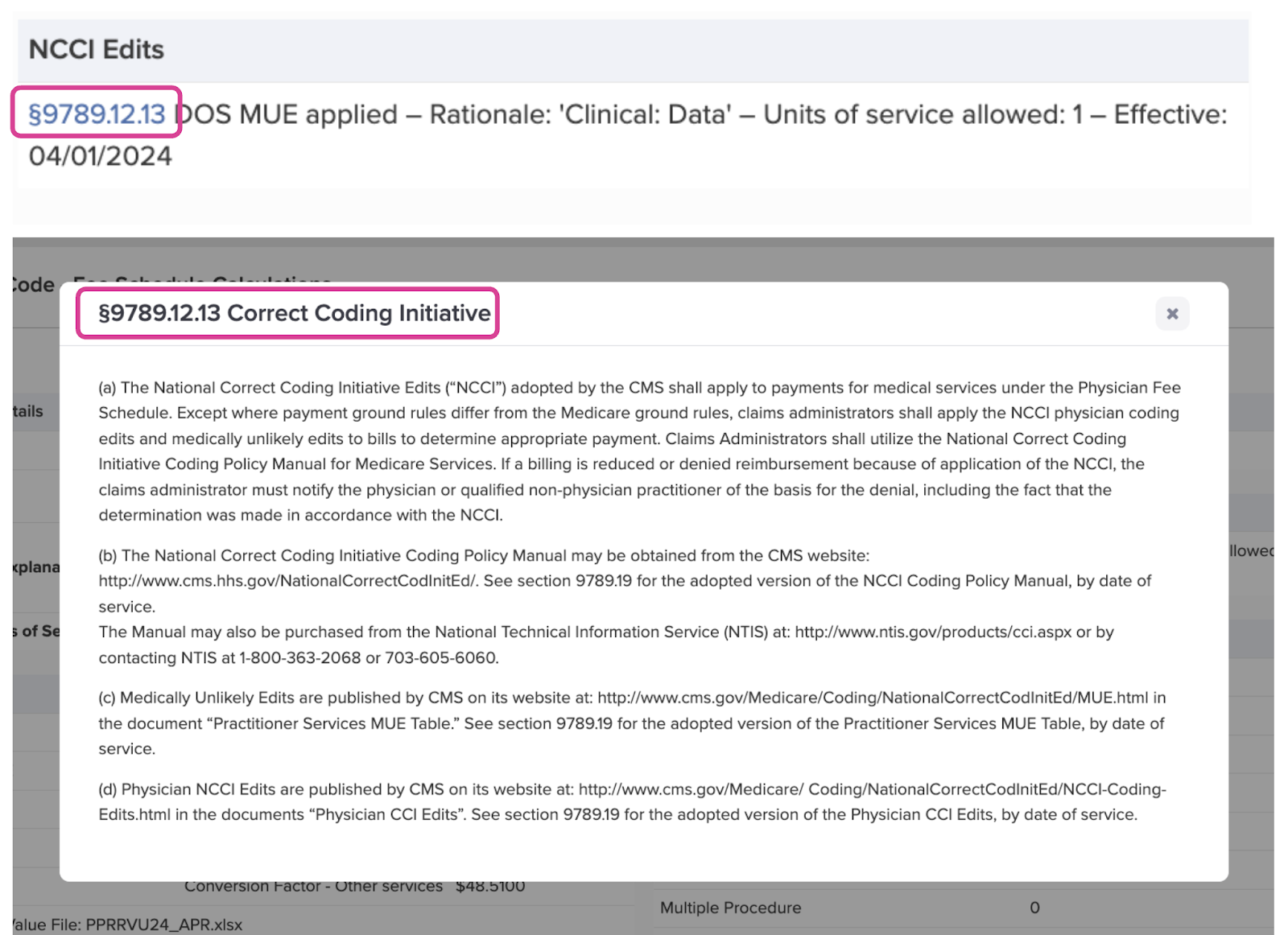
The daisyWizard goes a step further; by clicking the blue hyperlink on “§9789.12.13,” the user can see the specific regulation (shown below) indicating that NCCI edits apply.
Correct Is Correct (No Matter Who It Benefits)
Though our fierce advocacy for provider rights and payer compliance is undeniable, our goal is not (and has never been) to help providers at any inappropriate expense to insurers, employers, or Third-Party Administrators (TPAs).
Our goal is to provide the tools for a better workers’ comp system that efficiently heals injured workers and restores them to full lives and employment.
Willy-nilly calculations, cocktail napkin math, and best guesses based on PDF downloads of Medi-Cal rates can only create friction and drive even more providers away from treating injured workers.
Our ideal should be the shared vision of all stakeholders on both sides of the billing and payment equation: a system in which injured workers know they’ll be taken care of, employers know their premiums are well-spent, and doctors know they’ll be compensated appropriately per the applicable fee schedules.
In that scenario, everyone wins. All it takes is expertise and reliable technology, which daisyBill proudly delivers daily.
Know (and get) exactly what you’re owed for treating injured workers. See instant, accurate fee schedule calculations with daisyWizard’s Fee Schedule Calculator.
TRY THE CALCULATOR
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.
.gif)