Coventry Network: Non-Physician Providers Cost Less
Workers’ comp is in crisis. Doctors are fleeing the system, leaving employers and injured workers an increasingly smaller pool from which to seek care.
For doctors, the reasons to avoid workers comp are only too obvious: laborious authorization requirements, inane reporting demands, nightmarishly complex billing mandates, and (not least of all) networks seizing large percentages of the fee schedule reimbursements due to doctors.
Jill Harris — not uncoincidentally the Senior Vice President for Network Management at Coventry — recently penned an article with a proposed physician shortage “solution.” Ms Harris proposes improving access to care by expanding networks, and creating a larger pool of lower-paid non-physician providers who are allowed to treat injured workers.
But in proposing possible “solutions” to the doctor shortage, Coventry, a network entity, chose to ignore the obvious financial reason that doctors shy away from treating injured workers. Mainly, that Coventry and other networks reduce physician reimbursements to unsustainable levels.
Why Is There a Provider Shortage (Really)?
Writing for workcompwire.com, Harris correctly decries the overall provider shortage in health care generally, citing stats on the nationwide patient-to-provider ratio and reported burnout among health care professionals.
But instead of focusing on the challenges specific to workers’ comp, Harris conveniently lumps workers’ comp’s woes into the broader problems facing the health care industry.
Harris offers a look at the workers’ comp provider shortage through the lens of naked self-interest. The article reimagines the problem as one mostly caused by COVID and an aging population — rather than a refusal by providers to sink their practices by accepting the comically low reimbursement rates engineered by the likes of Coventry.
Providers are not refusing workers’ comp because of the elderly or the pandemic. While states establish fee schedules for treating injured workers, many states allow NETWORKS to impose — and subsequently lease — discount contracts that reduce doctors’ reimbursements to rates substantially lower than the fee schedules allow.
Doctors who flee workers’ comp are making a rational financial decision to refuse the sub-Medicare rates imposed on workers’ comp by networks, like Coventry.
Yes, the huge proportion of Americans over 65 and the undeniable effects of COVID have ripple effects across the health care space, including workers’ comp. But to end the analysis there is a lie of omission.
Coventry’s “Solutions”
Harris offers a list of four possible solutions that — while a potential boon for Coventry and its ilk — amount to nothing less than trading quality of care for quantity of care.
Harris’ recommendation is to allow more non-physician providers to treat injured workers. In her article, Harris cites states that allow “other providers,” like chiropractic assistants, to bill for workers’ comp services. Additionally, the article mentions jurisdictions that allow nurse practitioners and physician assistants to bill without a supervising physician involved.
Harris offers a 4-point plan to “save” workers’ comp. In addition to increasing the use of telemedicine (the only worthwhile suggestion in the article), Harris suggests:
-
Expanding the use of provider networks. Shockingly (not), Harris believes that expanded networks will increase access to quality and timely care. She writes: “...provider networks that expand with the regulations and demand for care will become a key resource to ensure injured employees have access to both timely and high-quality treatment options.”
Instead of expanding the networks, what if state legislators banned networks from reducing physician reimbursements to below fee schedule rates?
What if doctors were paid 100% of the state fee schedules? That would constitute a simpler solution to the simple problem that networks are reducing doctors’ reimbursements to an unsustainable level.
-
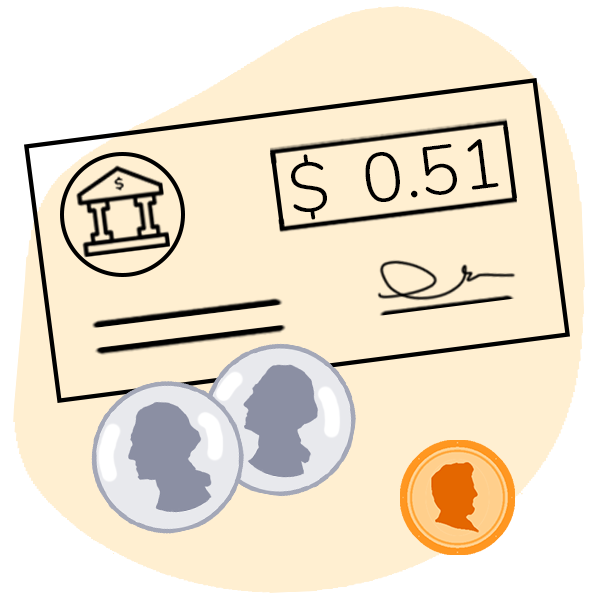
Leverage care management staff. Harris suggests utilizing case managers to direct injured workers to — prepare to be shocked again — network providers. Why? With an obligatory nod to “claim continuity” and care, Harris gets to the real point: better “cost outcomes.”
Harris fails to explain how better “cost outcomes” would encourage more providers to treat injured workers. Does Coventry believe non-physician providers will be more willing to accept the network reductions that often pay below Medicare rates?
-
And finally, just to add insult to non-compensable injury, Harris offers the final piece of the puzzle: “Ensure provider compliance.”
Putting aside the fact that in states like California, claims administrators “ensure provider compliance” by randomly denying any bill, Harris offers other ways to keep those pesky providers in line. Namely, the bluntly Orwellian suggestion that payers “look to their network partners to help educate providers…to help them comply.”
Harris’s manifesto of cheaper care for workers (and a tighter network grip on providers) is not an attempt to solve a problem.
It’s a shockingly tone-deaf, wildly un-self aware “let them eat cake” moment in which a network representative offers a system to treat injuries that, presumably, none of the C-suite executives at Coventry would accept for themselves or their families.
Missing from this missive is the real reason for the provider shortage in workers’ comp: regulatory red tape, bureaucratic inefficiency, and not least of all, the concerted effort by Coventry and other networks to drive provider reimbursement into the dirt.
Make workers’ comp a better investment. From fee schedule calculators to billing software to complete managed billing, DaisyBill has your back. Contact us to learn more.
LET’S CHAT
DaisyBill provides content as an insightful service to its readers and clients. It does not offer legal advice and cannot guarantee the accuracy or suitability of its content for a particular purpose.

.gif)